Key Takeaways
- Understanding Sleep Apnea: Sleep apnea is a sleep disorder characterized by interruptions in breathing during sleep. It can have serious health consequences if left untreated, including an increased risk of diabetes, heart attacks, strokes, and a shorter lifespan. It can also affect the quality of life due to disrupted sleep patterns.
- Surgical Treatment Options: Surgery is one of the treatment pathways for sleep apnea, but it’s typically considered when other non-surgical options like lifestyle changes, CPAP machines, or oral appliances have not provided sufficient relief. There are several surgical procedures available, each with its own benefits and risks.
- Variety of Surgical Procedures: The choice of surgery depends on individual factors like age, weight, medical history, and the severity of sleep apnea. Each procedure has its unique set of risks and success rates. Surgery may not always completely cure sleep apnea, but it can significantly improve symptoms in many cases.
Sleep apnea is a disorder that can not only disrupt your sleep cycle — it can also lead to serious health issues. That’s because sleep apnea actually impacts your breathing at night, causing it to periodically stop. This condition can be very serious and those suffering from severe or moderate sleep apnea might be recommended surgical therapy to ensure your airways remain unobstructed.
There are different treatment pathways that you might be offered to to treat mild, moderate, and severe sleep apnea. We’ll walk you through each of the most common types then explain how they work, recovery times, risk factors, and explain other options available to you.
Sleep Apnea: Definition, Risks, and How It Impacts Your Life
Sleep apnea is a sleep disorder where your breathing starts and stops throughout the night. Sleep apnea can be caused by a variety of factors, including excess weight or obesity. In fact, sleep apnea occurs in 3% of individuals within a normal BMI and 20% of individuals who are overweight. It occurs more often in men, but an increased risk appears to be for women following menopause.
There are three types of sleep apnea — obstructive, central, and complex. Obstructive sleep apnea (OSA) occurs when air is unable to flow through your passageways, due to an obstruction, while your body attempts to breathe. Often this airway blockage comes from excess tissue in the throat, but there are other potential factors such as nasal structure.
Central sleep apnea occurs when your brain does not send the signal to your muscles to continue breathing. Obstructive sleep apnea is the most common, while central sleep apnea affects less than 10% of patients referred to sleep laboratories, according to the American College of Cardiology.
Complex sleep apnea is when you suffer from both obstructive and central sleep apnea. Obstructive sleep apnea treatment includes a range of interventions such as lifestyle modifications, continuous positive airway pressure (CPAP) therapy, oral appliances, surgical options, and positional therapy, tailored to address the specific needs and preferences of the individual.
Nasal surgery is conducted under general anesthesia, with the majority of procedures lasting approximately one hour. There are surgical options for sleep apnea targeting the throat and tongue, including UPPP, Transpalatal Advancement Pharyngoplasty, TORS, hypoglossal nerve stimulation, tongue reduction, and partial epiglottidectomy. Individuals typically return home on the same day and experience complete recovery in about a week. a simple outpatient procedure.
For individuals with mild obstructive sleep apnea and small uvulas, a doctor might suggest Palatal Implants. In this procedure, a surgeon administers a local anesthetic to numb the throat and implants three small, stiff strips of plastic into the soft palate using a needle.
Meanwhile, radiofrequency volumetric tissue reduction (RFVTR) involves the use of a heated instrument to contract and firm the tissues in and around the throat. This procedure applies to the soft palate, tonsils, and tongue and is a way to treat those who cannot tolerate CPAP. Additionally, procedures like septoplasty and turbinate reduction aim to enhance nasal passage openness, thereby improving airflow.
No matter which type of sleep apnea you suffer from, if sleep apnea is left untreated, Verified Source Johns Hopkins Medicine University focused on medical research that produces thoroughly reviewed health articles. View source it can lead to severe side effects. These include type 2 diabetes, heart attacks, and other heart complications, strokes, and a shorter lifespan. In severe cases, it can lead to death overnight, though in most cases, sleep apnea’s symptoms will hurt your health over time.
Why Surgery Can Treat Sleep Apnea
Typical treatments for sleep apnea include:
- Lifestyle changes to decrease weight for better sleep
- Use of oral devices or a CPAP machine
- Preventing throat tissue collapse by switching to side sleeping
- Elevating the body with an adjustable bed or wedge pillow
If sleep apnea is more severe, a BiPAP machine may be used instead of a CPAP machine. At times, medications like steroids may also be prescribed. However, in some instances, surgical alternatives may be recommended.
There are many different surgeries available for sleep apnea, and reasons for recommending one can vary. For instance, if a sufferer isn’t seeing results from traditional treatments, then a surgical procedure may be considered. Your doctor will take your individual factors including age, weight, medical history, sleep apnea severity, and current treatment methods into consideration when deciding if you’re a candidate for surgery.
Individuals with severe obstructive sleep apnea may be advised by a surgeon to undergo a procedure that necessitates general anesthesia and hospital admission. Depending on your specific anatomy, a surgeon might suggest a combination of procedures.
While surgical procedures may be recommended for your sleep apnea, it’s important to understand that they’re not always successful in curing sleep apnea symptoms, though they can lessen them.
9 Common Procedures for Sleep Apnea
Here are ten of the most recommended surgeries for sleep apnea Verified Source Harvard Health Blog run by Harvard Medical School offering in-depth guides to better health and articles on medical breakthroughs. View source the risks to consider with these sleep apnea surgeries, and the success rates.
We should also note that since there are multiple potential underlying causes or risk factors for sleep apnea, some people may need to undergo more than one procedure. Many of the more invasive and extreme surgeries are done only after a previous surgery for sleep apnea has proved ineffective.
1. Radiofrequency Turbinate Reduction
 One way to treat sleep apnea is by reducing the size of the bones in your nasal cavity. Also known as turbinates, this bone structure and lining can be enlarged in spots, leading to obstruction when sleeping. In these cases, a turbinate reduction procedure may be recommended.
One way to treat sleep apnea is by reducing the size of the bones in your nasal cavity. Also known as turbinates, this bone structure and lining can be enlarged in spots, leading to obstruction when sleeping. In these cases, a turbinate reduction procedure may be recommended.
Risks include bleeding, scar tissue, infections, and can lead to something known as empty nose syndrome. While empty nose syndrome is rare, it can lead to discomfort, drying, crusting, and the feeling that your nose is blocked. Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source
While this surgery can be effective at improving your breathing, it’s not a guaranteed solution. While many patients experience reduced symptoms or no symptoms post-surgery, this procedure does not work for everyone.
2. Tonsillectomy and Adenoidectomy
 This procedure is an extremely common way to treat obstructive sleep apnea in children, as the cause is often enlarged tonsils. It can be used to treat adults in some rare cases. However, it’s typically not an effective solution for adults.
This procedure is an extremely common way to treat obstructive sleep apnea in children, as the cause is often enlarged tonsils. It can be used to treat adults in some rare cases. However, it’s typically not an effective solution for adults.
We should also note there are two types of tonsillectomy surgeries: lingual tonsillectomy and palatine tonsillectomy. Palatine tonsils are what we commonly call “tonsils” and are located on both sides at the back of the throat. Meanwhile, lingual tonsils are located at the back of the tongue.
If children have swollen tonsils or adenoids and suffer from sleep apnea, this procedure can provide relief and allow them to breathe better at night. Overall, tonsillectomy and adenoidectomy procedures are considered routine and safe.
However, risks of this procedure include a sore throat, the possibility of infection, and bleeding. Eating and swallowing will also be difficult for days post-surgery. In children, these procedures can be 75% to 100% effective in treating sleep apnea symptoms such as a child’s snoring, even if the child is overweight.
This can eliminate or improve sleep apnea to the extent that continuous positive airway pressure (CPAP) or other appliances become unnecessary.
3. Uvulopalatopharyngoplasty
 This is the most common procedure performed to help sleep apnea sufferers and is a type of soft palate surgery. A uvulopalatopharyngoplasty removes excess soft tissue from your throat, done to help widen the airway behind your tongue, shorten your soft palate, and allow air to flow better through your passageways at night. This surgery can be performed with a laser or with a radiofrequency probe.
This is the most common procedure performed to help sleep apnea sufferers and is a type of soft palate surgery. A uvulopalatopharyngoplasty removes excess soft tissue from your throat, done to help widen the airway behind your tongue, shorten your soft palate, and allow air to flow better through your passageways at night. This surgery can be performed with a laser or with a radiofrequency probe.
Risks of an uvulopalatopharyngoplasty include damage to the muscles of your soft palate and throat, velopharyngeal insufficiency (inability to prevent fluid from coming up through your nose), change in your voice, pain when swallowing or speaking (usually for the first few weeks), disruption to tastes, tongue numbness, or the development of silent apnea. With silent apnea, snoring is no longer an indicator of sleep apnea, but the airway problem remains.
While snoring is commonly cured by this procedure, only 40% of sufferers report a reduction or alleviation of sleep apnea symptoms.
4. Thyrohyoidopexy and Hyoid Suspension
 Thyrohyoidopexy and hyoid suspension are surgical procedures recommended for individuals with mild to moderate obstructive sleep apnea (OSA) and notable obstruction behind the tongue. This intervention involves repositioning the hyoid bone to pull the tongue forward, concurrently moving the tongue and epiglottis downward and forward.
Thyrohyoidopexy and hyoid suspension are surgical procedures recommended for individuals with mild to moderate obstructive sleep apnea (OSA) and notable obstruction behind the tongue. This intervention involves repositioning the hyoid bone to pull the tongue forward, concurrently moving the tongue and epiglottis downward and forward.
The hyoid bone is a U-shaped bone located in the neck that supports the tongue and helps maintain the structure of the upper airway.
During hyoid suspension surgery, the surgeon repositions and stabilizes the hyoid bone to prevent its collapse into the airway during sleep. This is achieved by attaching the hyoid bone to the thyroid cartilage or other structures in the neck.
Thyrohyoidopexy involves attaching the hyoid bone to the thyroid cartilage, similar to hyoid suspension. However, it may also include additional modifications to the surrounding tissues.
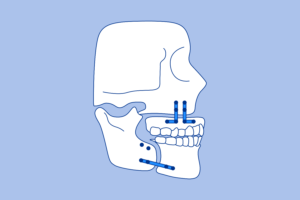
5. Maxillomandibular Advancement (MMA)
 A
maxillomandibular advancement
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
is often done by an oral and maxillofacial surgeon and requires fracturing both the upper and low jaw in order to move them forward and widen your airway.
A
maxillomandibular advancement
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
is often done by an oral and maxillofacial surgeon and requires fracturing both the upper and low jaw in order to move them forward and widen your airway.
This surgery can be extremely effective for sleep apnea sufferers, since the oral surgeon widens the airway at different points, starting at the nasal cavity to the hypopharynx. However, it’s often recommended after soft palate surgery has failed or proved unsuitable for a candidate.
Risks of this procedure include infection, teeth damage, nonunion of bones (when cut bones fail to heal together), mandible fracture, nasal obstruction (specifically one side of the nose), numbness in face, joint discomfort, and in less than 1% of patients, palatal necrosis requiring another operation. Healing takes about six weeks in total. You should expect changes to your face, though most patients report improvements in facial appearance.
This surgery is often successful at eliminating sleep apnea or significantly improving the symptoms for the majority of patients.
6. Anterior Inferior Mandibular Osteotomy
 This is another popular treatment method performed for sleep apnea sufferers. During an
anterior inferior mandibular osteotomy,
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
your chin is separated in two, which gives your tongue more room to move forward and can lead to an improvement in breathing during sleep.
This is another popular treatment method performed for sleep apnea sufferers. During an
anterior inferior mandibular osteotomy,
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
your chin is separated in two, which gives your tongue more room to move forward and can lead to an improvement in breathing during sleep.
On the downside, this procedure is not as effective as treating severe sleep apneas as maxillomandibular advancement surgery, particularly for obese patients.
7. Genioglossus Advancement
 This procedure pulls the tongue muscle attached to your lower jaw forward. A genioglossus advancement surgery
helps your tongue remain firm
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
during sleep and can prevent the blocking of air for sufferers of sleep apnea. A small screw or plate is inserted to hold the tongue in place with your lower jaw’s bone surface.
This procedure pulls the tongue muscle attached to your lower jaw forward. A genioglossus advancement surgery
helps your tongue remain firm
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
during sleep and can prevent the blocking of air for sufferers of sleep apnea. A small screw or plate is inserted to hold the tongue in place with your lower jaw’s bone surface.
In this surgical procedure, the chin bone is advanced along with the genioglossus muscle to prevent the collapse of the tongue onto the throat. The genioglossus muscle, linked to the underside of the chin, facilitates the movement of the tongue forward during contraction. This helps clear your upper airway. Risks for this operation include pain for up to two weeks, liquid diets, bleeding, risk of infection, and more.
While this procedure is less risky than others and has a shorter recovery period, it’s also not as effective at treating sleep apnea symptoms in all patients. This surgery typically has a 53% success rate, regardless of BMI. Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source
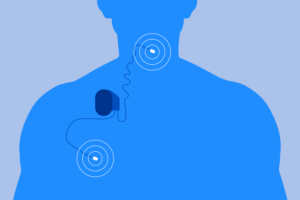
8. Hypoglossal Nerve Stimulator Surgery
 This relatively new procedure takes a different approach to treating sleep apnea. During the procedure, the
hypoglossal nerve stimulator
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
is surgically implanted in patients. This stimulator can sense the movement of your chest walls while sleeping, and can contract your genioglossus muscle, which causes your tongue to protrude. This allows air to flow more freely through the airway. Settings can be controlled by remote, allowing patients to turn this on at night and off in the morning.
This relatively new procedure takes a different approach to treating sleep apnea. During the procedure, the
hypoglossal nerve stimulator
Verified Source
National Library of Medicine (NIH)
World’s largest medical library, making biomedical data and information more accessible.
View source
is surgically implanted in patients. This stimulator can sense the movement of your chest walls while sleeping, and can contract your genioglossus muscle, which causes your tongue to protrude. This allows air to flow more freely through the airway. Settings can be controlled by remote, allowing patients to turn this on at night and off in the morning.
Infection and the migration of the device are the two most commonly reported side effects, but others can include Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source tongue stiffness or abrasion, discomfort, and swelling. Patients also recover faster than with other sleep apnea procedures.
While this procedure is still relatively new, studies show positive correlations Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source between this procedure and increased quality of life, brought on by decreased sleep apnea symptoms.
9. Tracheostomy
 During this procedure, an opening is cut into your trachea, just underneath your larynx. A
tracheostomy
Verified Source
Medline Plus
Online resource offered by the National Library of Medicine and part of the National Institutes of Health.
View source
allows you to breathe freely at night. During the day, this hole can be plugged, so you can talk normally. This operation is only used for very severe cases of sleep apnea that cannot be treated through other means.
During this procedure, an opening is cut into your trachea, just underneath your larynx. A
tracheostomy
Verified Source
Medline Plus
Online resource offered by the National Library of Medicine and part of the National Institutes of Health.
View source
allows you to breathe freely at night. During the day, this hole can be plugged, so you can talk normally. This operation is only used for very severe cases of sleep apnea that cannot be treated through other means.
While it’s considered 100% effective for sleep apnea, it will alter a sufferer’s quality of life and should not be done without the patient fully understanding the risks and ways they’ll need to adjust their lifestyle habits post-operation.
Additional Procedures for Sleep Apnea Sufferers
While the above are some of the top procedures for treating sleep apnea and its symptoms, there are other nasal surgeries or surgery for obstructive sleep, tongue procedures (such as tongue reduction surgery), and other operations that may be recommended for your specific sleep apnea symptoms.
By altering the anatomy and improving the stability of the hyoid bone, the procedure aims to reduce airway collapse and alleviate the symptoms of sleep apnea. The choice between these procedures depends on the surgeon’s expertise, the patient’s anatomy, and the specific goals of the intervention.
One more treatment is the Nasal valve surgery aims to widen and stabilize the internal nasal valves, situated directly behind the nostrils. If there is a structural cause, such as a deviated septum obstructing the airway, surgeons may suggest surgical intervention. With nasal surgeries, surgeons may employ cartilage from the nasal septum or another body area, nasal implants, or radiofrequency to reshape or reinforce this region.
Bariatric surgery, a procedure designed to induce weight loss, has the potential to alleviate sleep apnea in individuals dealing with extreme obesity. This type of surgery is typically recommended due to additional health risks associated with obesity.
Procedures can vary in complexity and recovery time, while risks also depend on the severity of the surgery.
Getting Diagnosed with Sleep Apnea
 If you think you’re suffering from sleep apnea and may require surgical intervention, talking to your doctor should be your first step. Your doctor will run your medical history, ask about your sleep behaviors, and may inquire about your family’s medical history before proceeding to recommend surgery with local anesthesia or in an operating room with general anesthesia.
If you think you’re suffering from sleep apnea and may require surgical intervention, talking to your doctor should be your first step. Your doctor will run your medical history, ask about your sleep behaviors, and may inquire about your family’s medical history before proceeding to recommend surgery with local anesthesia or in an operating room with general anesthesia.
From there, a sleep study is usually ordered, though other procedures like an electrocardiogram, may be conducted to determine if you’re suffering from sleep apnea. This usually is done in a sleep center, with sleep specialists monitoring your vitals throughout the night.
Nocturnal polysomnography involves being connected to equipment that monitors heart, lung, and brain activity, breathing patterns, as well as arm and leg movements, while also measuring blood oxygen levels during sleep.
A home sleep test could also be prescribed, though it typically will not collect as much information as a sleep study at a specialty center or laboratory. Still, you may need to do a home study first, to see if the results rule out or confirm sleep apnea or if further study is needed.
You may be referred to other doctors or sleep medicine specialists depending on the severity of your sleep apnea and your particular symptoms. Treatment recommendations will depend on your medical history, age, health, severity of symptoms, and other lifestyle factors.
Can Non-Surgical Treatments Help?
Most doctors will recommend nonsurgical treatments before turning to procedures to treat sleep apneas. If you’re overweight, changing your diet to lose weight will often be recommended. Increasing physical activity may also be prescribed, and (regular exercise is tied to better sleep, too). In some cases, this is enough to eliminate sleep apnea, if you’re able to keep the weight off.
Other treatments may include medications like steroids, particularly for those with allergies. Verified Source Medline Plus Online resource offered by the National Library of Medicine and part of the National Institutes of Health. View source Nasal steroids have been found to effectively reduce sleep apnea symptoms for many sufferers.
One of the most common treatments is a CPAP mask, or continuous positive airway pressure machine. This device sends air through your nasal passages while you sleep, keeping your airways open and preventing blockages. You’ll need to wear a mask connected to the CPAP device Verified Source National Library of Medicine (NIH) World’s largest medical library, making biomedical data and information more accessible. View source each night when you go to bed. While this treatment may seem difficult at first, it can be extremely effective at reducing or eliminating sleep apnea symptoms.
Oral appliances might also be prescribed to keep your tongue forward in your mouth, which also helps to keep your airways open. You may need to be fit for an oral device by your dentist in order to ensure a more comfortable experience while sleeping. Less commonly, sleepers may be advised to try mouth taping for snoring.
Lastly, in some cases, your sleep apnea might be caused by another medical issue, in which case, treating that disorder could eliminate your sleep apnea symptoms. For example, allergies can affect sleep apnea, though they are not a direct cause of sleep apnea. Taking steps to manage allergies can include:
- Sleeping on a hypoallergenic mattress
- Wrapping yourself up in hypoallergenic sheets
- Keeping warm with a hypoallergenic duvet during the cooler months
- Using a bed skirt to prevent dust and dust mites from collecting underneath the bed
- Looking into medication and natural remedies to manage seasonal allergies
Similarly, asthma can increase the risk of sleep apnea. You need to research tips for sleeping better with asthma to minimize the effects that respiratory issues can have on sleep apnea.
This may be as simple as not sleeping with a fan on. Or it may mean looking into ways to control your bedroom’s environment more thoroughly.
You may need to consider the benefits of an air purifier, which can trap many of the allergens that might trigger an asthma flare-up.
Similarly, you may need to be careful about your bedroom temperature for sleep, along with your room’s humidity. Cold, dry air can irritate people with asthma and worsen their symptoms.
“Careful treatment pathway needs to be considered which will then lead to optimize your health, daytime and cognitive functioning.”
Dr. Dagmara Dimitriou, Professor of Sleep Education and Research
Frequently Asked Questions
Can sleep apnea be cured by surgery?
Surgery can relieve sleep apnea, but it’s rarely the first treatment that doctors will recommend for sleep apnea. After all, surgery can be costly, come with complications, and may not even fix the issue.
Typically, less invasive treatments like CPAP machines, oral appliances, medications, and a new diet for weight loss are prescribed first to help keep your airway open. If these treatments prove inadequate, doctors may turn to surgery as a way to relieve symptoms.
Who qualifies for sleep apnea surgery?
Because there are many types of surgeries that can alleviate sleep apnea, the qualifications for each surgery will vary. For example, some surgeries may only be recommended if a person has severe sleep apnea that cannot be treated with CPAP therapy or an oral device. Surgery patients may also need to be a certain age
Talking with your doctor or speaking to a referred surgeon can help you better understand what options might work for you.
Can pediatric sleep apnea be treated with surgery?
Yes, surgery may be recommended for children with sleep apnea, though the exact surgery a doctor advises will depend on the root of the issue. For example, children who experience sleep apnea from overly large tonsils and adenoid tissue may have those removed. The removal of these blockages makes it easier to breathe at night.
Other types of surgeries, such as tongue base suspension, palate reconstruction, and nasal passage surgery, can relieve pediatric sleep apnea.
How long does it take to recover from sleep apnea surgery?
Since there’s no one surgery for sleep apnea, recovery time can range from a handful of days to a few weeks. Your age and genetics can also affect how quickly you heal after a surgery, along with how well you care for your surgical wounds. Speaking with your surgeon can give you a better idea of how long you’ll need to recover from a surgery for sleep apnea.
How can sleep apnea be treated non-surgically?
CPAP therapy is one popular way to relieve sleep symptoms without surgery. Oral appliances such as nasal strips can also be used during sleep, while performing exercises to strengthen mouth and throat muscles can prevent soft tissues from blocking a person’s airway. Losing weight can also help people with sleep apnea have a significantly easier time controlling symptoms.
The Bottom Line
There are many different surgical methods for treating sleep apnea, but all focus on improving your airway passages, so you can breathe easier at night. While some surgeries can be extremely effective at treating sleep apnea, they’re not without risks and should not be considered without weighing all of the pros and cons.
However, Professor Dimitriou adds that, “Living with sleep apnea should not be taken as an option but careful treatment pathway needs to be considered which will then lead to optimize your health, daytime and cognitive functioning.”
For this reason, many doctors recommend nonsurgical treatments first, seeking to improve sleep hygiene with lifestyle changes. Talk to your doctor if you have any questions about a particular procedure or to find out if you’re a good candidate for one of these treatment methods.
About the author
Courtney Johnston is a seasoned freelance writer and editor with over 10 years of experience in publishing digital content. Her areas of expertise include personal finance, small business, and health and wellness. With her work published in reputable outlets such as The Chicago Tribune, MSN, AOL, The Motley Fool, Benzinga, The Balance, Best Reviews, and The Culture Trip, Courtney brings a wealth of knowledge and a strong editorial background to her writing.
View all posts